Physicist, Heal Thyself
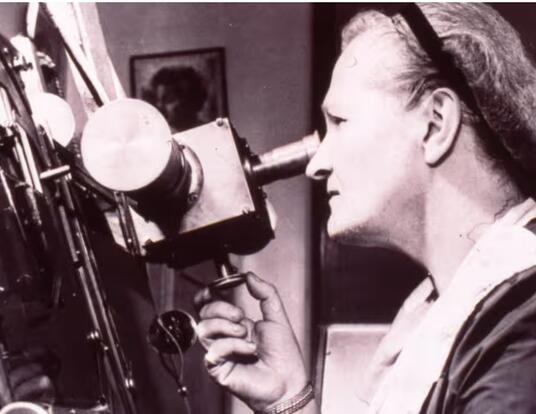
Nabiha Saklayen hopes to transform medicine with lasers and stem cells

When she was six years old and living in Bonn, Germany, a school assignment about planets ignited Saudi Arabian-born Nabiha Saklayen’s fascination with science. She wanted to learn more about astronomy, and her mother, Ferdousi Banu, an elementary school teacher, brought home “beautiful, very illustrative books,” Saklayen recalls. “That was my early introduction to physics, chemistry, and biology,” she says. “It was fascinating to me that there were so many scientific languages with which to view the world.” Over the years that followed, she came to love how physics in particular could be a “universal lens” through which other sciences might be understood. “Being trained in physics and math can be a powerful way to enter different realms of science.”
Today, Saklayen’s passion for using physics to explore other fields has brought her to a cross-disciplinary frontier. The 2017 GSAS PhD is the CEO and co-founder of Cellino, a Cambridge startup using laser physics, optical imaging, machine learning, robotics, and biology to develop a type of medicine that transforms the body’s own skin and blood cells into stem cells and then many other types of tissues that can be used for healing and repair. “Regenerative medicine,” she says, “will soon become a very important pillar in medicine overall.”
So far, no stem cell therapy has received the Food and Drug Administration’s approval. Two challenges bar the way: safety and scalability. To solve both, Cellino has created a robot laboratory to automate cell production and ensure quality, harnessing physics and other disciplines to make stem cell manufacturing safe, efficient, and affordable so millions of people can seek treatments that might, for the first time, reverse degenerative conditions.

Drive and Commitment
In 1989, when Saklayen was born in Riyadh, Saudi Arabia, her mother carefully chose her name. In Arabic, Nabiha means “eminent” or “intelligent.” Over the years, Saklayen’s dedication to her studies proved worthy of her name. Attending high school in Sri Lanka, she explored her interests—theater, creative writing, Model United Nations, and the Bengali music her mother taught her to play—even as she strove to master physics. “I love a good challenge, and physics was harder than math or chemistry or biology,” she says. Her love of challenges, she believes, comes from her mother. “Growing up, I saw her rising to challenges all the time,” she recalls. Born in a small town in northern Bangladesh, her mother was the first woman in her family to convince her parents to let her attend university—a decision to take risks that, Saklayen says, “directly translates into my journey and my opportunities.”
During Saklayen’s time in Sri Lanka, the 2004 Indian Ocean earthquake and tsunami struck, killing more than 35,000 nationally and 220,000 people worldwide. (In a twist of fate, Saklayen’s family canceled a beach trip because she was sick.) As deprivations and frustrations mounted, Sri Lanka’s civil war reignited after years of ceasefire. “There were a lot of suicide bombings happening in the part of the city where I was living and going to school and where my parents were working,” she says. “It was a tough time to be a teenager. In the back of your mind, you’re always wondering, ‘Am I in danger? Could something happen?’” At the dinner table, her family talked about making the most of every day. “My drive and commitment to my work and my education really crystallized while I was in high school,” she says.
During Saklayen’s senior year, she received a full scholarship to Emory University, where she majored in physics and minored in mathematics. She was drawn to biophysics, however, after losing her beloved grandmother to diabetes. “That was the first time I truly appreciated that medicine does not have all the answers yet,” she says. Saklayen made biophysics her focus when she enrolled at GSAS in 2012 so that she could help create tools that would support biologists and lead to new applications in medicine and cell engineering.
At Harvard, Saklayen developed laser- based methods to deliver cargo—such as molecules that edit genes—into cells. Cells are complex and sensitive, and penetrating them with foreign material often kills them if not done delicately. Using lasers, Saklayen made tiny bubbles to create temporary pores in their membranes, allowing cargo to enter. “At some point in the middle of my PhD,” Saklayen says, “my technology was taking shape, and I got very excited and started emailing biologists all across campus.” The multidisciplinary environment of Harvard’s GSAS, with dozens of graduate programs, was ripe for collaboration. “Everyone had a shared vision around working together to develop new technology to change science in a meaningful way,” she says. “That vibrant environment played a huge role in pushing me down this entrepreneurial path. I only had to walk across the street to talk to some of the best biologists in the world.”
It was miraculous to me that you could take an adult cell and add biological factors to it to bring it back to its embryonic-like state, which means the cell could then be turned into many different cell types.
Saklayen began envisioning new applications for her lasers after meeting Laurence Daheron, the head of the iPS Core Facility at the Harvard Stem Cell Institute. Daheron said that technologies were needed to engineer induced pluripotent stem cells (iPSCs), those from which all other cells grow. “I started to read the literature about induced pluripotent stem cells,” Saklayen says, “and I was blown away.” She was becoming aware of a revolution in biology set into motion in 2006 by Shinya Yamanaka’s lab in Kyoto, Japan. It showed that cells—when treated with four molecules naturally produced by the body—could be converted into pluripotent stem cells. “It was miraculous to me that you could take an adult cell and add biological factors to it to bring it back to its embryonic- like state, which means the cell could then be turned into many different cell types, such as neurons, retinal cells, heart cells,” Saklayen says.
Soon, Saklayen was collaborating with renowned biologists Derrick Rossi, assistant professor in the Stem Cell and Regenerative Biology Department at Harvard Medical School; David Scadden, the Gerald and Darlene Jordan Professor of Medicine; and George Church, the Robert Winthrop Professor of Genetics, who is now a scientific advisor for Cellino. Church recalls being impressed by Saklayen’s work. “She had a terrific vision of cells as the key therapeutic of the near future, the major challenges in cell therapy, and how to fix them,” he says. Once Saklayen had successfully tested her lasers on a range of cell types, including stem cells, she began contemplating a startup. Cellino was launched in 2017 after brainstorming sessions with her two co-founders: Matthias Wagner, a Harvard College graduate and serial entrepreneur specializing in optical technology, and Marinna Madrid, PhD ’18, her lab mate at Harvard.
“Meeting Marinna in graduate school was a pivotal moment in my life and my journey,” Saklayen says. “In college, I was usually the only girl in most of my physics classes. Then I got to graduate school, and it was really powerful to have a lab mate like Marinna. We were both women of color doing physics, and we worked so well together.”
As Cellino has grown, Madrid has seen the impact of having a company led by women of color. “Other folks from underrepresented minority groups feel more comfortable joining,” she says.
Cellino’s mission, however, didn’t come into focus until 2018, when Saklayen met with Bastiano Sanna, the then CEO at Semma Therapeutics and now head of cell and gene therapy at Vertex. “I was showing him this beautiful data of delivering cargo into cells,” she recalls, “and he said, ‘This is great. This is very interesting, but we’re really struggling—and we, as an industry, are struggling—to remove unwanted cells in cell cultures. Can your technology do that?’” The problem, which struck Saklayen as easy, led her to a realization: “Building a company is not about my interests. It’s about what partners need, what the industry needs, what customers need.”
From Artisanal to Automated
That seemingly simple task—removing unwanted cells—was in fact a Herculean undertaking so crucial to medicine that it became Cellino’s focus. Its importance lies in the risks and difficulties inherent in iPSCs. After cells are treated with biological factors, not all successfully convert, and scientists must remove those that don’t. “The primary way has been with a highly trained scientist sitting at a bench, looking at iPSCs under a microscope and using a pipette tip to scrape away unwanted cells by hand once a day, several times a day, for weeks, up to three or four months,” Saklayen says. “So, it’s very artisanal.” The job is not only taxing and expensive due to the time required but also demands extensive training. “Very few scientists know how to make iPSCs at very high quality.”
After the initial conversion, iPSCs are again converted either into retinal cells for age-related blindness or pancreatic cells to treat diabetes. Care is again taken to ensure that they are the right type, have no defects, and that no iPSCs remain since they carry the risk of becoming cancerous if put in the body. For early medical trials, patient-specific cells are required for 5 to 20 patients and can be handmade by a few scientists. “But as your clinical trials progress, you have to dose hundreds of patients,” Saklayen says. “Then, once the therapy is approved, you could get into thousands per year. There aren’t enough scientists who can make hundreds and thousands of batches of patient-specific cells by hand.”
It's not just that we’re women and people of color... we’re physicists trying to break into regenerative medicine. —Marinna Madrid, PhD ’18
To culture iPSCs safely and efficiently, Cellino’s team—comprised of 35 experts and counting—has combined knowledge from several disciplines to create a mechanized lab. “Our approach is to take this artisanal manual process and automate the various pieces,” Saklayen says. In their current prototype, one robot injects cells into custom well plates that another moves through the various stations before the plate is inserted into a machine that scans the cells and uses a laser to kill those that are unwanted.
A major focus at Cellino has been developing machine learning algorithms to identify which cells have successfully converted. “Our laser systems have single-cell precision, so you could, if you wanted to, remove individual cells or entire colonies,” Saklayen says. Cellino is developing a closed cassette approach, which is a significant innovation since, in the artisanal production of iPSCs, cells must be converted in high-grade clean rooms to prevent cross-contamination each time scientists work on iPSCs from a different patient. Cellino, however, will be doing imaging and laser removal of cells inside the cassettes. “If successful, Cellino technology will allow simultaneous manufacturing of multiple patient samples, hence reducing manufacturing cost and increasing the speed of running iPSC therapy trials,” says Kapil Bharti, a senior investigator at the Ocular and Stem Cell Translational Research Section at the National Institutes of Health.

Saklayen’s team aims to have the automated closed-cassette system ready for market by 2025. With the goal of starting its FDA interactions next year, Cellino hopes to participate in trials with Bharti and others at the NIH in the future. “The patient populations we’re looking at for our first two products—age-related macular degeneration and Parkinson’s—they’re massive,” Madrid says. In the United States alone, 11 million people have age-related macular degeneration and 1 million have Parkinson’s. For age-related macular degeneration, which causes blindness, Cellino will create retinal cells, and for Parkinson’s, it will make dopamine- producing neurons. Small early trials have already shown promise for therapies treating these diseases as well as diabetes and epidermolysis bullosa, a rare inherited condition causing fragile skin. But numerous degenerative diseases—involving every organ—might also be treated. “For us, as an industry, we’re dreaming about cures,” Saklayen says.
Today, even as Cellino expands, it is an outlier. “I don’t see other biotech companies in Boston led by two women of color, and I think that’s really special and powerful and indicative of the future, which is going to be very exciting as people from different walks of life, with different perspectives, enter biotech to create paradigm shifts that will hugely benefit patients,” Saklayen says. “And it’s not just that we’re women and people of color,” Madrid points out, “but we’re physicists trying to break into regenerative medicine.” As outliers in the world of biology, Saklayen, Madrid, and Cellino itself are in many ways the products of the GSAS’s multidisciplinary melting pot.
When Saklayen looks back on her journey, she sees that physics has in many ways served her well as a universal lens, allowing her to explore across disciplines, finding novel solutions to create new therapies.
“Over the next 10 years, we’re going to see many of these therapies hit the finish line. This is a phenomenal time,” she says. “It’s going to change the world."
Photos by John Soares
Get the Latest Updates
Join Our Newsletter
Subscribe to Colloquy Podcast
Simplecast