Getting the Upper Hand on Malaria
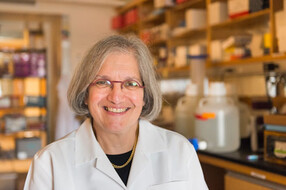
Dyann Wirth leads an integrated team of PhD students, clinicians, and public health experts to eradicate a stubborn enemy
Research at Risk: Since World War II, universities have worked with the federal government to create an innovation ecosystem that has yielded life-changing progress. Now much of that work may be halted as funding is withdrawn. Find out more about the threats to medical, engineering, and scientific research, as well as how Harvard is fighting to preserve this work—and the University's core values.
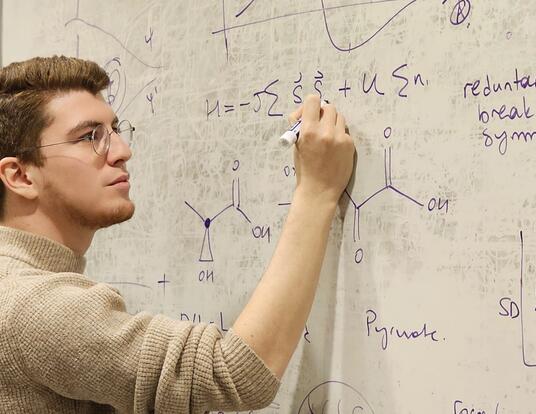
Daria Van Tyne bends over a crimson disc, her gloved hand swinging the tip of a pipette in circles to agitate a mixture of substrate and human blood that fills the petri dish. It’s not apparent, but she’s a foot soldier in a war that has been raging for decades. With the press of a trigger, the red mixture is drawn up, and with it thousands of single celled parasites. These are Plasmodium falciparum, the deadliest of several Plasmodium species that cause malaria.

Van Tyne is a GSAS PhD student in the Wirth Lab at the Harvard School of Public Health, part of a large team of graduate students, postdocs, faculty, and clinicians led by Dyann Wirth, chair of the Department of Immunology and Infectious Diseases. The lab is the epicenter of the global fight against malaria, conducting groundbreaking explorations of the Plasmodium genome and developing technologies to identify the mechanisms responsible for the parasite’s wily adaptability. It is at the scientific vanguard of a new push to eliminate those Plasmodium species that cause 216 million cases of malaria and an estimated 655,000 deaths each year, according to the World Health Organization. An old disease, less headline-grabbing than Ebola or bird flu, malaria nonetheless places a dramatic burden on the health and economies of countries — some of the poorest in the world — where it is ingrained.
Wirth and her students stand out among their peers for having a strongly integrative understanding of malaria. Their collaborators — from Harvard, the Broad Institute, and labs and treatment centers around the world — include molecular biologists, geneticists, computational biologists, chemists, statisticians, and epidemiologists. Wirth knows it’s not simply a parasite she and her colleagues must contend with. On the genetic side of things, there are human host, parasite, and mosquito vector genomes in play. At the political level, there is a parasite that ignores country borders and demands cooperation among neighbors. And then there are the technical, economic, and logistical concerns: how to get what is needed (bed nets, medications, vaccines) where it needs to be when it needs to be there. “Realistically,” says Wirth, “this is a 50-year project.”
Getting the Root of Resistance
The previous push to eradicate malaria worldwide — after World War II, spurred by the discovery of the game-changing drug chloroquine, and on the heels of successful eradication in the American Southeast — can best be described as carpet-bombing. (Military metaphors seem de rigueur in any discussion of the malaria problem.) Drugs were distributed liberally, swamps were doused in pesticides, and no heed was paid to a fundamental facet of evolution. “We were putting a tremendous amount of pressure on malaria,” Wirth says — on the parasites that cause it and the mosquitoes that deliver it. But the harder you try to eradicate a species, the more evolutionary impetus there is for it to evolve and develop ways to survive. The only lasting effect of the carpet-bombing, it turned out, was widespread drug resistance in the malaria parasites and insecticide resistance in their hosts. As Wirth puts it, we were in a battle with the disease and suddenly found that “the bullets no longer worked.”
At present, there is only one bullet left that is fully effective: artemesinin, introduced in 2005. There are no fallbacks should resistance to this drug become widespread. Plasmodium, we now know, has tremendous variability in its genome and in its capacity to reproduce and recombine genetic material very quickly, both of which lend it an evolutionary nimbleness that makes brute medicinal force highly ineffective.
“We still have the same two tools [antimalarial drugs and insecticides] that we had in the 1950s,” explains Wirth. So what do we do? “Understanding the parasite and its biology is critical,” she says. Her lab has identified areas of the Plasmodium falciparum genome with markedly lower variability than the rest. These areas are likely to have been subjected to some very powerful evolutionary force — such as that instigated by the previous eradication effort. Indeed, lab members have already identified the gene responsible for the chloroquine resistance that rendered previous efforts moot, and they are using this method to suss out more of the secrets of the parasite’s resistance.
Now the team hopes to identify burgeoning resistance early enough to give clinicians time to change their approach. Rachel Daniels, another PhD student in the lab, uses the genomic data to study the population structure of the parasite. Scientists can get an idea of transmission rates, for example, by looking at the rate of recombination of genetic material in a given population. Knowing where transmission is especially high could yield policies to coordinate limited resources and prevent the rapid spread of resistant populations.
An Integrated Team, A Complex Foe
This work is very much a team effort. Van Tyne spends a large part of her time tending to the needs of these cultured parasites — a process she describes with cheerful irony as “pampering.” If she leaves the petri dishes alone, even for a weekend, the cultured parasites could outstrip the available resources in the dish and kill themselves via overpopulation.

In a chamber downstairs, an insectary is breeding mosquitoes for use in experiments to better study malaria transmission. Inside, the air is thick: warm and humid. Cloth cages teem with mosquitoes, and rack upon rack of shallow dishes hold their fidgety, comma-shaped aquatic larvae.
Meanwhile, other members of the Wirth Lab are picking apart the genetic identity of Van Tyne’s charges, sequencing the DNA of numerous individual parasites and pulling together a picture of the entire Plasmodium falciparum genome. The lab takes samples each year from the field, from a clinic in Senegal, so that the malaria parasites they work with are as close to their natural state as possible.
In nature, the parasites spend their lives inside one of two hosts: human or Anopheles mosquito. When an infected mosquito draws blood, a spore-like form of the parasite hitches a ride in the mosquito’s saliva. Inside the human body, those parasites move straight to the liver, where they set up shop safe from the human immune system. They multiply asexually, and once this liver population reaches critical mass — days or weeks or months later, depending on the parasite species and the individual infection — a new crop of parasite cells, merozoites, enters the bloodstream and begins to invade red blood cells. One parasite to a cell, they clone themselves again and again, until a terrible act of coordination brings them all bursting out of their red blood cells to begin another cycle of infection. This time, a much larger number of parasites infects a much larger number of red blood cells.
In humans, the Plasmodium cells reproduce only clonally. A given infection is essentially the same individual parasite reproduced to the size of population. Eventually, some of these individuals break out of the asexual loop, transforming into male and female gametocytes (sex cells) and entering the bloodstream to wait for the lucky bite of a mosquito. It’s only once they’re in a mosquito’s gut that the parasites reproduce sexually, gaining the potential to reshuffle their own genetic material or combine it with that of another individual-population.
This complicated life cycle is both a boon and a burden to the war effort. It makes rearing malaria in the lab particularly tricky, but it offers numerous targets for intervention. The problem is coordinating these efforts. For instance, “if we bottleneck the parasite at transmission, what if the parasite becomes much more effective at being transmitted?” asks Wirth. At this point, she explains, many of the challenges are civil and societal ones. We have the tools to kill the parasite and control its vector. What we haven’t had is an integrated approach.
For example, Sri Lanka went from a handful of cases in 1963 to a million in 1985, says Wirth. Governments and policymakers don’t necessarily understand malaria’s potential for explosive growth and don’t have a grasp of its biology.
When a country has all of a half-dozen cases, she explains, it’s easy to see why its leaders might decide there are more pressing problems than malaria. Funds dry up.
“For people in malarial regions, it is a fact of life. The notion of eradication is radical,” says Wirth. (As Van Tyne puts it: “Malaria’s been around forever and a half.”) A big part of the challenge is convincing people that this is a disease that can be conquered, not a permanent feature of their landscape. As such, Wirth’s lab frequently hosts visitors from other countries and collaborators who can shed light on the local realities of trying to implement new methods of malaria control. Daniels cites, for instance, the challenge of convincing Buddhist populations in malarial regions that killing mosquitoes en masse might be permissible for the sake of public health.
Collaborative Life Sciences
This fall, Wirth will begin a tenure as chair of the Harvard Integrated Life Sciences program, a consortium of PhD programs in the life sciences meant to foster collaboration across departments. This seems a natural progression for a woman who has a singular talent for bringing together people from all walks of science and life to wage war on one of humankind’s oldest epidemics. “If you were to sit down and draw a tree of malaria researchers, it’s amazing how many of them come back to Dyann,” says Daniels. But Wirth rejects the spotlight: “Graduate students are critical to any scientific endeavor, but particularly in this area where there’s still so much unknown, and the technology is changing very rapidly.”
In spite of the turbulent history of eradication efforts and the sheer resilience of the malaria parasite, she is steadfast in her optimism. “The current state is hopeful. We are at a very important time — we can now demonstrate that this is a curable, treatable disease,” says Wirth, a four-star general mapping out her battle plan.
Photo by Ben Gebo
Get the Latest Updates
Join Our Newsletter
Subscribe to Colloquy Podcast
Simplecast