Striking Out Lou Gehrig’s Disease
Harvard Griffin GSAS Voices: Stanley Gill, PhD ’24
Research at Risk: Since World War II, universities have worked with the federal government to create an innovation ecosystem that has yielded life-changing progress. Now much of that work may be halted as funding is withdrawn. Find out more about the threats to medical, engineering, and scientific research, as well as how Harvard is fighting to preserve this work—and the University's core values.
Stanley Gill is a researcher at Arbor Biotech, a Cambridge-based firm that “develops programmable DNA editors with the power to enable creation of curative genetic medicines for patients.” Gill discusses his PhD research on amyotrophic lateral sclerosis (ALS), how growing up in a family of engineers eventually brought him to neuroscience and biology, and his time volunteering with a Harvard program that brings science to students at underserved Boston schools.
Researching Rare Ailments
I study rare diseases. During my PhD, I researched ALS, also known as Lou Gehrig’s disease. ALS is a disease of the motor neurons—the cells in your body that allow for coordinated control of muscular function. Motor neurons are connected to your spinal cord up to your brain and you use them to do anything physical including breathing.
With ALS, these motor neurons begin to die, resulting in gradual loss of voluntary function, eventual paralysis, and death. It is a devastating disease that progresses very quickly once you start to lose neurons, and there is no cure. It is also a very difficult disease to research because we have so few motor neurons, and those neurons we do have are essential for daily functioning. For example, the number of motor neurons between your head and foot that allow you to kick a ball or wiggle your toes could be as low as five. Furthermore, because motor neurons do not regenerate, we can’t take a sample from a living person and study them directly.
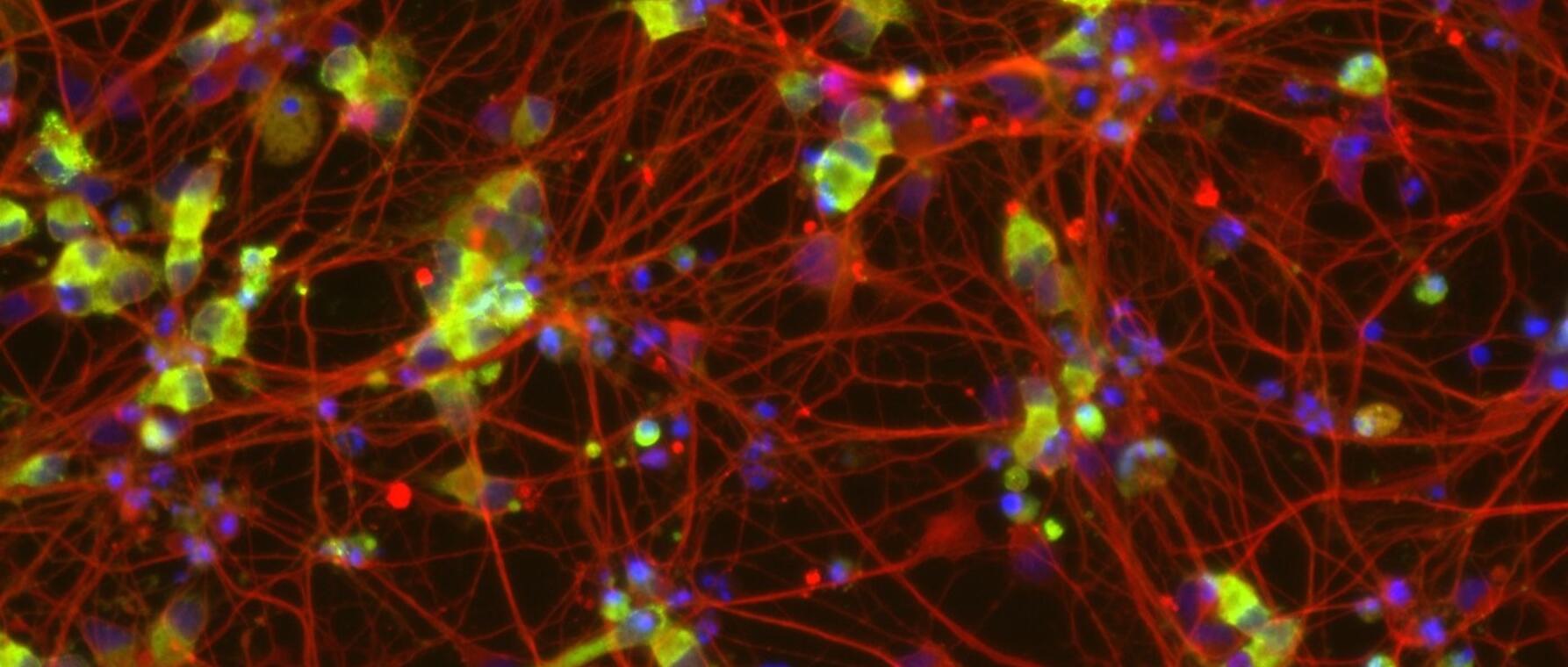
To get around this problem, I used stem cell-derived motor neurons. You could think of stem cells as the base version of cells compared to more specialized types like muscle or blood cells. Every cell in your body starts from a stem cell.
We can leverage stem cells’ potential to make neurons we can grow in a dish. We can also genetically modify stem cells to express and/or correct genes important to the onset and progression of ALS and compare how neurons with those changes live and behave. For instance, we took skin cells, which are plentiful and do regenerate, reprogrammed them to revert to stem cells again, and then turned those stem cells into motor neurons we could study.
One protein I focused on as a comparison point between these different experimental conditions is called TDP-43. It normally lives in the nucleus of the motor neuron, but in ALS-affected neurons it ends up outside. I created a human stem cell-derived motor neuron model to show the impact of the change so researchers could use it to find therapies and treatments for ALS in the future. Much of what I do today at Arbor Biotech, where we also study rare diseases, is built on the skills I learned at Harvard Griffin GSAS.
An Engineering Mindset
My parents studied industrial engineering for their undergraduate degrees, so naturally I was raised with an engineering mindset. I was a kid who wanted to take things apart, find out how they worked, and hear the full explanation of why and how something functioned. When I showed up at the Massachusetts Institute of Technology as an undergraduate, I thought I would be an electrical engineer. I quickly realized that humans were more complicated than robots and was fascinated by how electricity interacts with our brains. I wound up studying bioengineering.
That interest in taking things apart and discovering what makes them tick is good for both science and engineering. I want to know what the system is, which is science, and I want to know how we could make the system better, which is engineering. Sometimes I don’t know what all the pieces in the system are, or I don’t know what they do. Figuring that out is basically what every biologist does.


Hard Science, Soft Skills
While in graduate school, I ran the Health Professionals Recruitment and Exposure Program (HPREP). HPREP is a student-run volunteer initiative that invites high school students from underserved high schools in the greater Boston area to come to Harvard Medical School for a 10-weekend winter program. They attend supplemental lectures on topics in biology and biomedicine, including demonstrations from medical students on vital signs and physiology, and receive one-on-one time with graduate students who walk them through topics such as the college application process, applying to summer programs, networking, and more. They learn a lot of professional soft skills.
When I first joined HPREP, I was just another volunteer. Eventually, I became an executive director and oversaw the program during the COVID-19 pandemic. I was delighted when we transitioned to an online format and served even more kids than before. I have talked to the directors and leaders of programs similar to HPREP at other schools, and they tell me that our version of HPREP was one of the most organized and comprehensive, which goes to show that it was something that people at Harvard cared about building and growing for the long term. I give a lot of thanks to those who came to HPREP before me. I am so proud of what it has achieved.
Get the Latest Updates
Join Our Newsletter
Subscribe to Colloquy Podcast
Simplecast



