Changing Fate
How New Research in Cell Reprogramming Holds Hope for Type 1 Diabetes Treatment
Research at Risk: Since World War II, universities have worked with the federal government to create an innovation ecosystem that has yielded life-changing progress. Now much of that work may be halted as funding is withdrawn. Find out more about the threats to medical, engineering, and scientific research, as well as how Harvard is fighting to preserve this work—and the University's core values.
Ask the average person about diabetes and they’ll probably answer that it has something to do with eating too much candy or being overweight. For people living with type 1 diabetes, these myths mask what is for them a daily grind of blood glucose monitoring, insulin shots, and hyperawareness of diet that quite literally keeps them alive.
Type 1 diabetes, unlike type 2, is an autoimmune disease in which the immune system targets and destroys the insulin-producing beta cells in the pancreas. Without insulin, the body can’t control the level of glucose in the blood generated through diet. People with type 1 must monitor their blood sugar levels regularly throughout the day, adjusting diet and administering insulin as necessary. The more they check, the better they manage the disease—some only a few times a day, others many more. And that disease management can change over the years, with many developing complications—for example, hypoglycemia unawareness, which prevents people from sensing dangerously low levels of blood glucose.
Raise the idea of a cure, however, and people with type 1 diabetes are skeptical. “When I think of the word cure as it relates to type 1 diabetes, I get excited and annoyed at the same time,” says Anna Floreen, outreach manager at the T1D Exchange—a Boston-based organization dedicated to improving the lives of people touched by type 1 diabetes by driving faster, better research, and improving the quality of care. “On one hand, I can’t wait for the day of no finger pokes, insulin pump site changes, and that constant worry and guilt that not having ‘good enough’ control may lead to a future of complications and physical limitations. On the other hand, as someone who was diagnosed nearly 30 years ago, I feel really skeptical when I see news promising yet another cure.”
The Future Is Plastic
Researchers across Harvard are conducting research aimed at managing—or even curing—diabetes. And their approaches are as varied as the disease itself. Doug Melton, Xander University Professor and co-director of the Harvard Stem Cell Institute, uses human embryonic stem cells to develop insulin-producing beta-cells. Denise Faustman, director of the Immunobiology Laboratory at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, is testing a vaccine that may improve or even reverse the disease. Rohit Kulkarni, a senior investigator at Joslin Diabetes Center and professor of medicine at Harvard Medical School, explores why the immune system attacks the body and how to regenerate the beta cells it destroys.
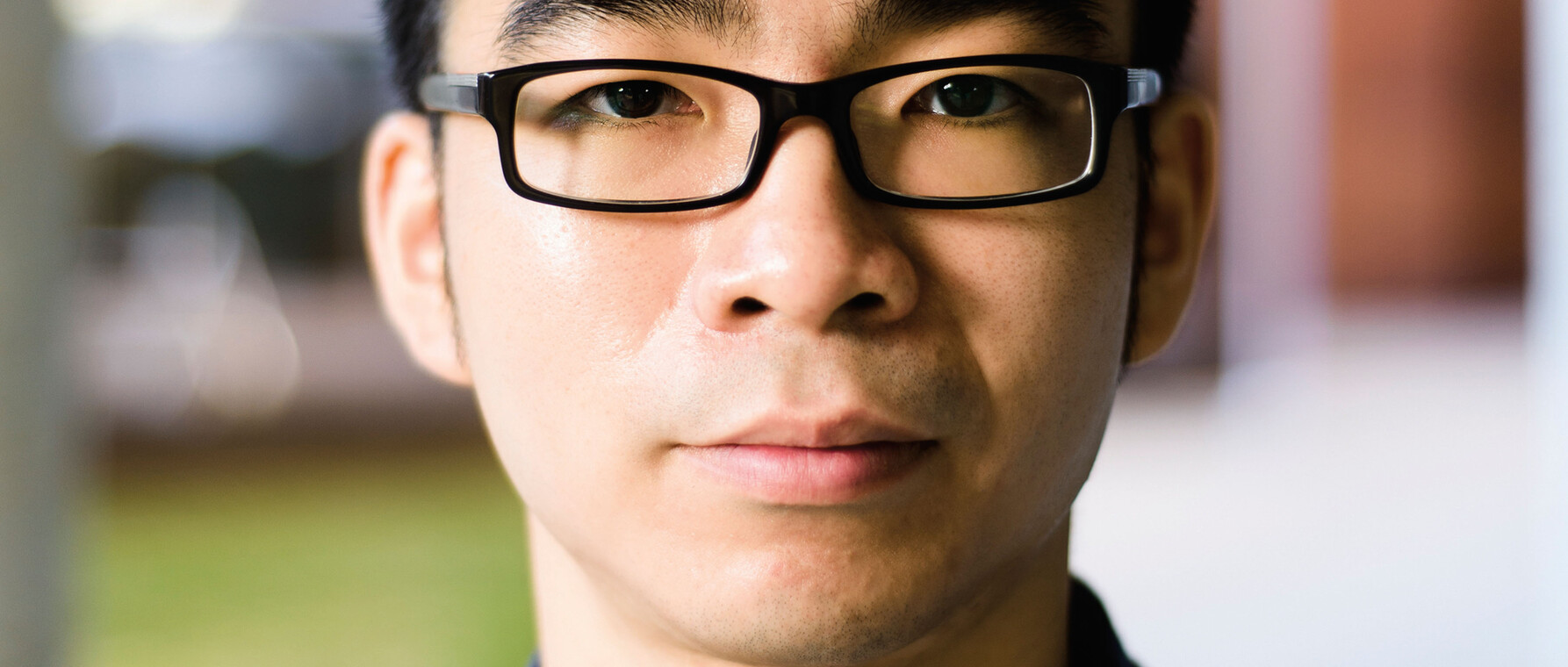
It is this work on beta cell regeneration that attracted PhD candidate Ivan Valdez to Kulkarni’s lab. Growing up in South Texas, Valdez watched members of his family and friends in the wider Hispanic community cope with the effects of type 1 and type 2 diabetes. He knew he wanted to help and first considered becoming a medical doctor. But as an intern at Weill Cornell Medical College through the Minority Biomedical Research Support Research Initiative for Scientific Enhancement (MBRS-RISE) program, he realized that he wanted to move in a different direction. “I always had an interest in the scientific method and in problem solving,” he shares. “But during MBRS-RISE I got carried away with medical research.”
As a first-year PhD student in biological and biomedical sciences, Valdez took a class that introduced him to the work of Shinya Yamanaka, the Japanese scientist who won the Nobel Prize for discovering how to turn a mature human cell into a stem cell—called induced pluripotent stem cells. “When I heard about Yamanaka’s work, I knew that I wanted to conduct similar research,” remembers Valdez. “After researching the principal investigators operating on the Longwood Campus, I discovered that Professor Kulkarni conducted research on my two interests, diabetes and pluripotent stem cells.”
The overarching focus of Kulkarni’s lab is beta cell regeneration, since beta cell loss unexpectedly occurs in patients with type 1 diabetes. “The beta cells are still trying to replicate and function, and finding therapies that aid this process while suppressing the autoimmune response is an important approach to the problem,” Kulkarni explains. “By increasing the number of insulin-producing beta cells by even 10 to 20 percent, we can better control the disease.”
Valdez helped advance this work during his first two years as a graduate student. But as he began considering options for his thesis, he decided to bring a new idea to Kulkarni: pancreatic plasticity. “Pancreatic plasticity is a very new area in diabetes research,” he explains. “The idea is that the cells within the pancreas are plastic, in the sense that they can convert from one type of cell into another type of cell.” The pancreas contains endocrine beta cells that generate the hormone insulin, which regulates the body’s blood sugar. It also contains exocrine cells, whose function is to secrete enzymes into the small intestine. Valdez decided to target the exocrine tissue and successfully demonstrated that they could be coaxed to transform into insulin-producing beta cells. Valdez described this achievement in an article that has been recently accepted for publication in the journal Cell Reports.
“That’s an aspect of graduate students I love; no matter where you are in your career, you can still learn from them because they ask out-of-the-box questions. It’s amazing how they keep me on my toes.”
For Kulkarni, Valdez’s initiative in trying something new is the best part of working with graduate students. “Ivan was excited about regeneration and after talking with others in the lab, he developed his own project that tackled a new idea in the field,” says Kulkarni. “That’s an aspect of graduate students I love; no matter where you are in your career, you can still learn from them because they ask out-of-the-box questions. It’s amazing how they keep me on my toes.”
Valdez cautions that while he has demonstrated that other pancreatic cells could be enlisted to produce insulin, these basic-science results need to be applied by other investigators and in human cells. And other factors need to be taken into account as well. “We have to learn how to control this plasticity,” he says. “It’s exciting to derive beta cells from other cell sources, but some of the mechanisms activated are also reported to occur, not surprisingly, in cancer where cell growth is a constant phenomenon. Researchers need to take this into account when moving forward.”
Changing Fate
When Chaiyaboot Ariyachet arrived at Harvard to begin his PhD in biological and biomedical sciences, he didn’t have a specific project in mind. His academic studies at Bowdoin College and at school in his native Thailand had focused on biology, and he wanted to continue his science research. As he participated in rotations early in his graduate-student career, he considered joining smaller, recently-established labs, where he could be involved more directly in the research and with the principal investigator. Then, he found the lab of Qiao Zhou, an associate professor in the Department of Stem Cell and Regenerative Biology, whose work in the field of regenerative biology and regenerative medicine concerned cell reprogramming.
Zhou investigates how to regenerate insulin-secreting beta cells as a potential treatment for type 1 diabetes patients, as well as those with severe forms of type 2. While Valdez exploits pancreatic plasticity, Zhou’s reprogramming approach uses genetic information to induce other cells in the body to become insulin-producing cells.
“His work in manipulating cell fate is pioneering,” says Ariyachet. “Converting one cell type into another, especially in adults, is really exciting.”
Each cell type in our bodies has a different function, guided by genetic information. Zhou discovered that by creating a cocktail of three specific genes expressed in the developing pancreas, he could induce an exocrine cell to produce insulin. Over time, the cells become more and more like beta cells, and eventually cluster together to form structures similar to the Islets of Langerhans.
The cocktail didn’t work only on pancreatic cells, however. Any cell could be reprogrammed to produce insulin. Working with Zhou, Ariyachet began wondering whether some cells would be more responsive than others.
“We used a mouse-model that contained these reprogramming genes and looked to see where insulin was being produced in the body,” Ariyachet explains. “We found that the gastrointestinal tract, specifically the pylorus region, is particularly amenable to insulin production.”
The pylorus, the area where the stomach opens into the small intestine, seemed an odd location for beta cell reprogramming, so much so that it had never been considered as a candidate before. “Actually, if you look closely at the development of the stomach, especially the pylorus, it’s closely related to the pancreas,” explains Ariyachet. “It arises from a common pool of progenitors.”
Using pylorus cells as a starting point, Ariyachet collaborated with David Mooney, Robert P. Pinkas Family Professor of Bioengineering at the Harvard John A. Paulson School of Engineering, who provided a biometric scaffold. Ariyachet added tissue to the scaffold and implanted it in the mouse’s abdominal cavity. Soon, cells formed and eventually created a “mini-stomach” that began producing insulin, essentially serving as an internal, organic insulin pump.
The structure had an added benefit: regeneration. “In the gastrointestinal tract, adult stem cells renew the gut epithelial cells every four to five days,” he says. “We were able to tap that process in the mini-stomach as well.” When they tested what would happen if they destroyed the first reprogrammed cells, they discovered that the local stem cells sprang into action and created more, a huge advance for a disease that nearly eradicates beta cells not so easily replaced.
We need more young people, unafraid of challenges, not bound by dogmas, to devote their time, energy, and life to tackling this disease, and we need the means to support them. Then the cures will come.
Zhou credits Ariyachet with making very important contributions to his research program. “His recent study on reprogramming gastrointestinal tissues into beta cells has led us down a new path,” he says. “He deserves much credit for tackling a challenging project and, through his hard work and creativity, bringing it to fruition.” Zhou’s lab is currently working on developing a human version.
While Ariyachet continues to conduct research on human stomach stem cells, he’s moved from mini-stomachs to a broader approach that simply converts cells into insulin-positive cells that can be constantly replenished. “When gut epithelial cells die, they are replaced with new ones for the rest of our lives,” he says. “The problem with type 1 diabetes is that insulin-positive cells are attacked by the autoimmune system. In this case, if you constantly produce an insulin-positive cell, it doesn’t matter. If they are destroyed, you can make more.”
The Challenge Ahead
With excitement building among investigators regarding the innovative research occurring in the type 1 diabetes space, it’s hard not to hint at the idea of a cure. But tackling, once and for all, such a complex and devastating disease requires dedicated scientists taking unique approaches. “Major scientific breakthroughs are needed for this disease, and true to all major scientific breakthroughs, one needs scientific minds with great creativity who think outside the box,” says Zhou. “We need more young people, unafraid of challenges, not bound by dogmas, to devote their time, energy, and life to tackling this disease, and we need the means to support them. Then the cures will come.”
Photos by Ben Gebo
Get the Latest Updates
Join Our Newsletter
Subscribe to Colloquy Podcast
Simplecast