How Lungs Heal
Understanding how cells interact and regenerate could lead to better treatments for cancer, COVID-19

Research at Risk: Since World War II, universities have worked with the federal government to create an innovation ecosystem that has yielded life-changing progress. Now much of that work may be halted as funding is withdrawn. Find out more about the threats to medical, engineering, and scientific research, as well as how Harvard is fighting to preserve this work—and the University's core values.
“In this refulgent summer,” said the philosopher, writer, and theologian Ralph Waldo Emerson at Harvard in 1838, “it has been a luxury to draw the breath of life.” Withdraw “refulgent” and Emerson’s words could well have applied to the summer of 2020, although with a very different meaning. Breathing freely—in many ways and for many different people—has become the great luxury of 2020.
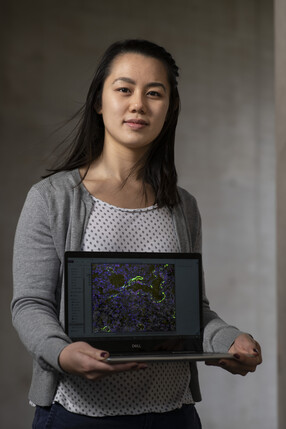
In that context, Irene Wong is a scientist for our time. The fourth-year PhD student in Biological and Biomedical Sciences at Harvard’s Graduate School of Arts and Sciences studies the way our lungs work. Specifically, Wong wants to get a better understanding of how cells interact to help damaged lungs heal and regenerate.
“My hope for this research is that it will provide a basic lens to understand the biology of lung function,” Wong says. “If you merge the translational and basic research then you can get a more holistic understanding of disease and develop better treatments.”
The “Main Player”
To date, much research has centered on the epithelial cells of the lungs—and with good reason. The epithelium not only lines the respiratory tract from the nose down to the bronchial passages, moistening the air and protecting the lungs but also is “the main player” in gas exchange and breathing.
“If we start with inhaling, the air needs to flow through these passages that are made up of epithelium,” Wong explains. “They bring air to more distant regions of the lungs, which is lined with epithelium that facilitates gas exchange.”
When we inhale, we also take in all the particulates and gases in the air. Pollution, respiratory illnesses like pneumonia, and cigarette smoke all damage or even kill the different types of cells in the lungs, making it more difficult to breathe.
“When you get a respiratory illness, it can cause damage to the epithelium,” Wong explains. “Usually, those cells regenerate, but when you have a long-term disease—say, from smoking every day for 10 or 20 years—damage accumulates. Some cells may mutate and pass on their mutations when they propagate, which is how lung cancer starts.”
In the case of COVID-19, caused by the SARS-CoV-2 virus, some of the worst damage can actually result from the body’s natural attempts to fight off the virus.
“The coronavirus SARS-CoV-2 infects the cells of the lungs,” says Wong. “When those cells become infected, not only do they die but also they can trigger a massive immune response. In a viral infection like COVID-19, it can cause a lot of long-term damage to the tissue if the balance of cell types and biological processes are not restored.”
Cellular Communication
In the fight against diseases like COVID-19 and lung cancer, researchers in the Kim Lab at Boston Children’s Hospital, where Wong works, are learning more about the epithelial stem cells that repair damage to the lungs. Carla Kim, professor of genetics and pediatrics at Harvard Medical School and the principal investigator of the Kim Lab, points out that that stem cells don’t operate in isolation.
“Cells in each of our organs talk to each other,” she says. “These cell-cell interactions are critical for how our tissues are maintained and how they receive signals when something is going wrong.”
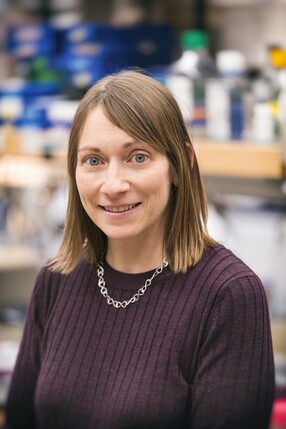
Kim and her team want to test the hypothesis that some diseases occur because something has gone wrong with the way that cells interact. Right now, scientists don’t really know which of the more than 40 different cell types in the adult lung can make more of themselves and which can’t but might have the ability to send signals and factors that help in regeneration.
“In the lung, mesenchymal cells make connective and other types of tissue that support the organ,” Kim says. “Sometimes they’re dividing. Sometimes they’re secreting. Sometimes they’re providing structural support. But they’re pretty understudied and we need to know more about them.”
Kim says that Wong’s work builds on recent research that shows adjacent mesenchymal cells secrete proteins and other factors that help with epithelial cell regeneration. Mesenchymal cells also have demonstrated their own stem cell-like behavior, expanding and giving rise to others.
“What it boils down to is, ‘Can any cell divide and make another cell?’” Kim says. “We think that only stem cells have that ability. We think that a fully differentiated cell doesn’t have that capacity and we wouldn’t call it a stem cell. A better understanding of the lung’s mesenchymal cells and the way they interact with the epithelium could form the basis of new therapies for respiratory diseases.”
Many kinds of mesenchymal cells exist, however, and it's unclear whether they really can self-renew or differentiate—or how they help epithelial cells to do so. Wong hopes to determine which cell types are most important for regenerating the lung’s airway. In particular, she wants to know if some mesenchymal cells are affected by injuries and, if they are not, how they help facilitate the lung’s regeneration.
“It hasn’t been fully established, within the lung field, which mesenchymal cells are damaged or lost with injury,” she says. “So, I’m looking at them more closely, as well as what role they play in how lungs heal.”
Although Wong does not work directly on COVID-19, Kim says that her work will enable clinicians to better understand how that disease—and many other respiratory illnesses—cause long-term lung damage and, perhaps, how to repair it.
What it boils down to is, ‘Can any cell divide and make another cell?’
“How are the mesenchymal cells different in the lung of a person that’s been infected with SARS-CoV-2 (COVID-19)?” she asks. “Does it damage the lung or change how it can respond to a future injury? Data are emerging showing that people who have recovered from the coronavirus might have some lasting damage. We’re not sure about that yet. So, one thing we’d like to do is to create a better model to study this. Irene’s work is part of that effort.”
A Commitment to Teaching and Mentoring
Wong could hardly find a better mentor than Kim, a pioneer in the use of stem cells to study lung cancer and pulmonary disease. But Wong says that it wasn’t only Kim’s brilliance and groundbreaking research that attracted her to the lab at Children’s: It was her commitment to teaching and mentoring young people.
“I wanted to work with someone who was really invested in student training,” she says. “In Professor Kim, I have someone who’s willing to step back and put me in touch with the resources I need to figure things out on my own. I’m in a lab environment where I’m supported by all my fellow colleagues. I’m very lucky.”
Wong shares Kim’s commitment to service—and to getting young people from diverse backgrounds involved in science. The daughter of working-class immigrant parents from China, Wong discovered the Continuing Umbrella of Research Experiences (CURE) program at Boston’s Dana Farber Cancer Institute, not far from her family’s home in Malden, Massachusetts. The internship program "introduces Massachusetts high school and college students from underrepresented populations to the world of cancer research...to encourage students to pursue future careers in the biosciences...." The experience changed Wong’s life—something she hopes to do for others like her in the future.
“The internship made me appreciate programs that reach out to high school students like me who come from underrepresented groups,” she says. “Depending on what school system they’re in, they might not have the kind of mentor they need. In an ideal world, students from all backgrounds would see at an early age that they’re capable of doing science.”
As a teaching fellow in the introductory undergraduate course Molecular and Cell Biology 64: Cell Biology in the World, taught by Professor Robert Lue and supported by Preceptor Jessica Liu, Wong tries to pass on the kind of support and encouragement that brought her into the sciences. She says that the effort to reach out to young people and diversify the sciences will be a priority for her long after she has her PhD.
“In order to address the systemic issues in higher ed from graduate school and upwards, there needs to be more outreach in high school and earlier,” she says. “I’m still thinking about what I can do to help with that when I graduate.”
Turning back to her research, Wong says that, like nearly everyone else in the world, she wants to see an effective treatment for COVID-19. She wants her work to contribute to that effort. But she also hopes it has a broader impact.
“There are a number of respiratory diseases that don’t have effective treatments yet—not just COVID-19,” she says. “If we were to understand the basic mechanisms of how different cell types in the lung work, then we could probably create more targeted therapies for specific diseases.”
That development would allow people around the world to breathe easier.
This research was funded by the National Heart, Lung, and Blood Institute and the National Institute of General Medical Sciences.
Illustration by Angus Greig. Photo of Irene Wong by Tony Rinaldo. Photo courtesy of Carla Kim.
Get the Latest Updates
Join Our Newsletter
Subscribe to Colloquy Podcast
Simplecast