The Kids Aren’t Alright
Stress & Development team studies impact of the coronavirus pandemic on youth mental health

Research at Risk: Since World War II, universities have worked with the federal government to create an innovation ecosystem that has yielded life-changing progress. Now much of that work may be halted as funding is withdrawn. Find out more about the threats to medical, engineering, and scientific research, as well as how Harvard is fighting to preserve this work—and the University's core values.

“What is this going to do to the kids?” That’s the question Dr. Alexandra Rodman, Dr. Maya Rosen, and Steven William Kasparek asked one another as the coronavirus pandemic forced lockdowns around the world.
Rodman, PhD ’18, and Rosen are postdoctoral research associates at Harvard’s Stress & Development Lab (SDL). Along with Kasparek, a PhD student in clinical psychology in the lab, they understood that the developing psyches of children were particularly vulnerable to the stressors that would follow from closed schools, sick or worried parents, and in-home isolation.
They were particularly concerned about the decrease in social interaction children normally get in class and with friends. They also wondered how families would cope with job losses or with worries about the health of family members who were frontline workers. And, of course, what if a loved one fell ill or even died? “We thought that the stress of the pandemic would have a real impact on the mental health of children and adolescents both now and over time,” Rodman says.
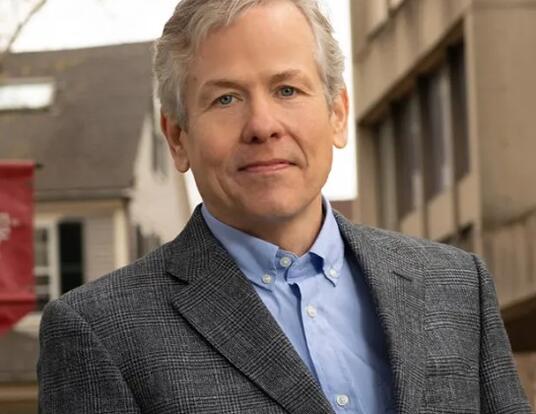
To understand the psychological mark COVID-19 has left on young people, Rodman, Rosen, and Kasparek began a longitudinal study under the direction of John L. Loeb Professor of the Social Sciences Katie McLaughlin. Their results indicate that the pandemic and its by-products of isolation and disconnection have indeed taken their toll on youth mental health. But the research also identifies behaviors that can mitigate the effects of the lockdown and help young people cope with stress long after the coronavirus has subsided.
Two Patterns

In April 2020, Rodman, Rosen, and Kasparek administered two exhaustive surveys—one for the youth and one for their caregivers—to about 220 families in the Seattle, Washington area for whom they had extensive data on mental health prior to the pandemic. They asked a total of 160 questions about their lives and current stressors related to the pandemic. Had someone lost a job? Had someone gotten sick? Did the children feel isolated or lonely? Was the family experiencing food or housing insecurity? Was the living situation tenser with people cooped up at home during lockdowns?
From the answers, the team created a “stress composite score” to measure the cumulative impact of the stressors in a child’s life, collected initial results in the spring, and then looped back in November 2020 to see how things had changed. McLaughlin, the study’s principal investigator, says the data confirmed the team’s initial concerns: Psychopathology dramatically increased among study participants during the pandemic.
“Two very clear patterns emerged,” she says. “First, mental health problems increased for kids during the pandemic. The proportion who reported clinically meaningful symptoms of depression, anxiety, or behavior problems doubled in our sample from about one-third of kids before the pandemic to two-thirds of kids after. The second trend was that the strongest predictor of these problems is how much exposure to pandemic stressors a family faced. The more the stressors accumulated, the more likely a child was to experience an increase in mental health problems.”
The concerns about social isolation that inspired the study were validated by the research. Rodman says young people reported a dramatic decline in in-person socialization during the pandemic that left them feeling more lonely and disconnected, a situation that improved but persisted over time.
“Feelings of social isolation decreased slightly between the spring and the fall of 2020,” she says. “The improvement was statistically significant, but it’s unclear how meaningful it was in the lives of the kids. They still reported feeling lonely and disconnected six months after the initial survey.”
Seattle, where the study’s participants live, was one of the first cities affected by the pandemic. The municipality instituted a strict lockdown that required homeschooling and also had a dramatic impact on its economy. Rosen says that stressors from both those aspects of the pandemic response showed up in the data.
The proportion who reported clinically meaningful symptoms of depression, anxiety, or behavior problems doubled in our sample from about one-third of kids before the pandemic to two-thirds of kids after.
—Professor Katie McLaughlin
“Kids were having trouble doing schoolwork at home,” she says. “It was hard for many of them to find a quiet place to learn or do assignments. Parents were often home because they had lost a job. Even if they were still employed, many suffered tremendous financial losses during the pandemic. As a result, we saw the stressors of housing and food insecurity as well.”

Taken together, the accumulated stress overloaded many developing psyches. Kasparek points out that the pandemic is particularly difficult for those going through adolescence, a time when social life is even more critical for well-being and identity, and also when mental illness typically starts to manifest. Moreover, young people lack the brain maturation and life experience that together enable adults to look past the present-day crisis with hope for better times in the future.
“The pandemic is tough for adults,” he explains, “but we’ve been through adversity in the past and have come out the other side. We're able to think forward more, to weigh the pros and cons of the current situation. Adolescents aren't able to think in the same way; it is more difficult for them to imagine a better situation even months or weeks into the future, let alone the 14 months that the pandemic has been going on. As adults, it’s hard for us to grasp what it’s like to be in that developmental life stage, even though we’ve all been through it.”
Buffers: The Pandemic Slayers
At a time when there is much speculation about the negative effect of social media on youth mental health, one of the surprising findings of the SDL study is that digital socialization might have “buffered” young people from the pandemic’s isolation. Rodman says that the level of online interaction reported by kids in November 2020 was more or less the same as it was in April and before the pandemic. But those who did experience an uptick in digital socialization also reported lower levels of psychopathology.
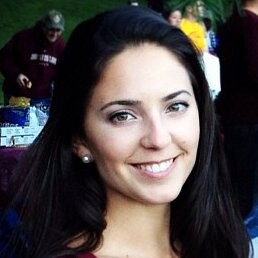
“It appears that young kids maintain somewhat lower levels of digital socialization,” Rodman says. “Adolescents, on the other hand, were already at a ceiling of digital socialization before the pandemic. During COVID, these levels remained stable on average for both groups, but variability shows up within each. Some kids engaged more after the pandemic began. Some less. We found that those who did engage in more digital socialization were protected from psychopathology related to stress.”
Rosen observes that less screen time also buffered against psychopathology, however, depending on how much news the kids were viewing and whether their time online was active or passive.
“Children and adolescents who had high levels of stressors during the early part of the pandemic had high levels of psychopathology both in April and when we resurveyed in November,” she says. “But those who engaged in less passive screen time overall—scrolling through social media or watching YouTube videos, rather than active digital socializing—were buffered against that association, both early and late. That’s also true for young kids, but not adolescents, who consumed less than two hours of news media per day.”
Being outside in nature didn’t help as much as the researchers thought it might, but having a stable daily routine did, even if it was different from the pre-pandemic norm. Exercise, as much previous research has shown, also buffered against the effects of stress.
“Physical activity had a buffering effect,” Rosen explains. “Kids who engaged in more exercise early in the pandemic showed lower levels of internalizing psychopathology. Those same kids who engaged in higher levels of physical activity early on were also protected from the impact of high levels of stress on psychopathology in later months.”
Rodman, Rosen, and Kasparek say that stressors decreased moderately across the board between the initiation of the study in April through the collection of follow-up data in November. Moreover, the behaviors that provided protection early on were still effective months later. Unfortunately, high stress scores measured in the spring still predicted pathology late in the fall, indicating that the pandemic may have a lasting effect on youth mental health.
We found that those who did engage in more digital socialization were protected from psychopathology related to stress.
—Alexandra Rodman, PhD ’18
Will the kids be alright? Rosen says only time—and further research—will tell if young people cope with the legacy of the pandemic in ways that are adaptive or maladaptive. Kids are resilient. Even those who experience poverty, neglect, and violence often learn to adapt. But what’s adaptive in one set of circumstances can be maladaptive in another.
“It’s hard to know how kids growing up now will respond when the pandemic’s over,” Rosen says. “Hopefully, this research will advance our understanding of vulnerability during times of crisis and provide families with some simple things they can do to protect their children and promote good mental health.”
Banner courtesy of Creative Commons
Get the Latest Updates
Join Our Newsletter
Subscribe to Colloquy Podcast
Simplecast