As Below, So Above
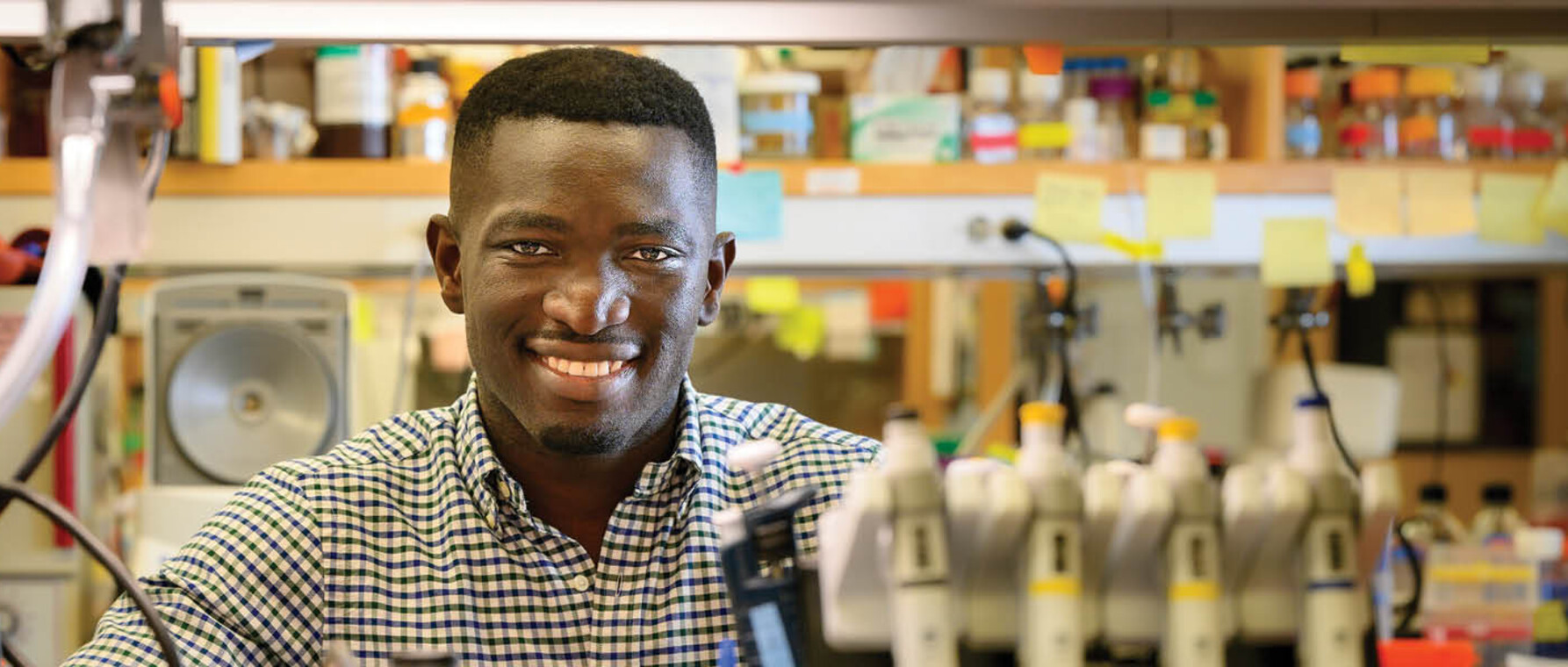
MD/PhD student Chidi Akusobi casts his gaze at microbes and the stars in the service of human flourishing
Research at Risk: Since World War II, universities have worked with the federal government to create an innovation ecosystem that has yielded life-changing progress. Now much of that work may be halted as funding is withdrawn. Find out more about the threats to medical, engineering, and scientific research, as well as how Harvard is fighting to preserve this work—and the University's core values.
Chidi Akusobi wrapped his fingers around the edge of the rock and lifted. Underneath, worms, pillbugs, and many other insects darted and wriggled. The young man was enthralled. He had discovered an entire community of life in his family’s Bronx, New York, garden. He wanted to study it, to observe, to discover its secrets of life. So, much to the chagrin of his mother, a nurse, he did what any budding young scientist would do. He tried to recreate the subterranean colony under controlled conditions at home.
“I got some Tupperware and filled it with dirt,” the microbiologist remembers. “I put some of the insects in there with leaves and some water, thinking that’s what they would eat. I checked every day to see if they were still alive. That was me at 10 years old.”
If, in the daytime, Akusobi looked down at the life on the ground, at night he looked up at the stars. “I was a curious child,” he says. “And one of the biggest things that inspired my curiosity was looking up in the night sky and asking, ‘What else is out there?’”
A student in the MD/PhD program of the Graduate School of Arts and Sciences and Harvard Medical School, Chidi Akusobi still spends a lot of time looking down at tiny living things. As a soon-to-be physician-scientist, he gazes through the lenses of powerful microscopes on the trail of new therapies for the treatment-resistant infections caused by the Mycobacterium abscessus. But as a recent participant in NASA’s Aerospace Medicine Clerkship program, Akusobi still keeps one eye on the stars—and on the future—contributing to the effort to make humankind a space-faring species.
Obsessed With Abscessus
If you’re not familiar with Mycobacterium abscessus, chances are you’ve heard of its close relative Mycobacterium tuberculosis (TB), the cause of one of the most deadly infectious diseases in human history. Like TB, abscessus infects the lungs but also other parts of the body, including skin, soft tissue, and blood. Moreover, while abscessus is less deadly than its bacterial cousin, it grows much faster and can live in a multitude of environments—water and soil—while TB requires a human host to survive. Finally, infections caused by abscessus are far harder to treat than tuberculosis. “You have to be on antibiotics every day for a year to two years, and even then, you still may not be cured,” Akusobi notes.

People who are immunocompromised or who have an underlying lung condition like cystic fibrosis are particularly vulnerable to abscessus infection. For that reason, Akusobi’s PhD advisor, Eric Rubin, director of the Rubin Lab at the Harvard T.H. Chan School of Public Health and editor-in-chief of The New England Journal of Medicine, says that abscessus is one of the rare infectious diseases that is more prevalent in wealthy countries than in the developing world.
“Because we’ve done a very good job of controlling TB in the US, infections caused by abscessus and its relatives are actually more common than TB here,” Rubin says. “Infections caused by ‘nontuberculous mycobacteria’ appear to be on the rise. And, for most, our therapies are very poor. Patients require years of therapy and most still are not cured.”
While abscessus is not as lethal as TB, the fact that it is so difficult to treat makes it a significant cause of morbidity, particularly among those with underlying conditions. Even when patients are otherwise healthy, abscessus infections can be debilitating.
“If patients have a soft tissue infection, then they may experience redness, swelling, and pain at the site,” Akusobi says. “If it gets worse, patients might start seeing pus and drainage from that site, characteristic of abscess formation. For lung infections, patients may experience increased mucous production, shortness of breath, and, over time, may even start coughing up blood. Patients can also feel the effects of systemic infection like fever, night sweats, and weight loss.”
Abscessus is so difficult to treat because of the thick, waxy cell wall that makes it hard for antibiotic drugs to penetrate and kill the bacterium. Even when medicine does get through, however, the bug has other lines of defense.
For most, our therapies are very poor. Patients require years of therapy and most still are not cured.
—Eric Rubin
“The bacterium encodes many, many genes that allow it to counteract the effects of drugs,” Akusobi says. “So, for instance, they have efflux pumps that push the drugs out as soon as they get in. They have enzymes that can deactivate drugs so that they are rendered useless. They can also evolve resistance to antibiotics by mutating antibiotic targets”
Akusobi’s work on abscessus enabled him to fulfill his ambition for his PhD: to ask a clinically relevant question and conduct research that advances understanding of the fundamental biology of a pathogen. For Akusobi, that question was, “What genes are responsible for conferring abscessus’s increased resistance to antibiotics?”
To answer that question, Akusobi screened around 5,000 genes and identified nearly 400 that were essential for the bacterium’s growth and survival. One gene in particular—penicillin-binding lipoprotein or PBP lipo—was critical for the proper growth and division of abscessus cells. Furthermore, Akusobi found that when the levels of PBP-lipo were reduced, abscessus became vulnerable to a range of common, cheap, and easily tolerated antibiotics, including ampicillin and amoxicillin.
“All of a sudden abscessus is now sensitized to drugs it was previously resistant to,” he says. “By reducing PBP-lipo’s levels, we ushered in a whole new class of antibiotics to treat abscessus. Moving forward, if we can find a way to target this gene, we could potentially make treatment cheap, well-tolerated, and more effective.”
Rubin says that it’s always hard to assess the ultimate impact of basic science. It takes many steps and many years to develop a new drug. At the same time, he’s optimistic that Akusobi’s research could be a step on the path to new, more effective therapeutics for the treatment of abscessus infections.
“We hope that some of the older drugs might affect the function of the protein that Chidi has identified,” he says. “We are currently trying to see if this is true with Chidi’s protein and a variety of other similar potential antibiotic targets.”
The Family Business
Just as Akusobi’s forays into the subterranean world of the family garden was only half of the story of his passion for science, so too his work as a microbiologist is only part of his education and career path. As soon as he received his PhD from GSAS in 2020, Akusobi returned to Harvard Medical School for the last two years of his MD degree, which he expects to complete in May 2022. He says that, in some ways, serving others through medicine is the family business.
“I come from a medical family,” Akusobi says. “Both my parents are nurses. My sister’s a nurse. I understand the joy that being of service to your fellow humans can bring. I also understand the limitations of medicine, and part of why I so enjoy research is I get to work on problems that address those limitations and push treatments forward for those who need them most.”
Akusobi also wants to be a doctor for the “one-on-one” connection with patients and the ability to have a direct impact on their lives—to see them get better through the application of science.
“I chose to get an MD and a PhD because I wanted to use and generate scientific knowledge to help people,” he says. “I think being a physician-scientist and having a real sense of what medicine can do for patients is important.”
Although abscessus infections are more prominent in the developing world, Akusobi says that his choice to focus on the treatment of infectious disease stems from growing up in a West African family.
“My family comes from Nigeria, where I was born,” he says. “In West Africa, infectious diseases like malaria, TB, and HIV are some of the leading causes of death. Being a doctor who specializes in that area is a way to use my passion for science to give back to my community.”
Space Doc
Given Akusobi’s research focus on the molecular level and his practical desire to work with underserved communities, his choice to take part in NASA’s Aerospace Medicine Clerkship program may seem unexpected. But it’s actually in line with a mind that is constantly questioning and filled with wonder for how the universe—whether inside the human body or beyond the limits of the Earth’s atmosphere—functions and evolves.
"I was always curious about space,” he says. “As time went on and I learned more about the planets, our solar system, and the galaxy, it only became more intriguing. I realized there are so many questions waiting to be answered.”
To help answer the questions that have to do with human biology, medicine, and space exploration, Akusobi joined the Space Medicine Operations team for a four-week program that included “formal lectures on space medicine topics and issues, familiarization with the medical aspects of International Space Station operations, design, and function as well as Exploration Medical Capability for deep space exploration.” (Sadly, his cohort had to work remotely rather than at the program’s headquarters at the Johnson Space Center (JSC) in Houston, Texas, due to the ongoing pandemic.) He and his colleagues were also required to complete a research project. Akusobi chose to study the way that NASA tests astronauts’ lung function during training.
As time went on and I learned more about the planets, our solar system, and the galaxy, it only became more intriguing. I realized there are so many questions waiting to be answered.
—Chidi Akusobi
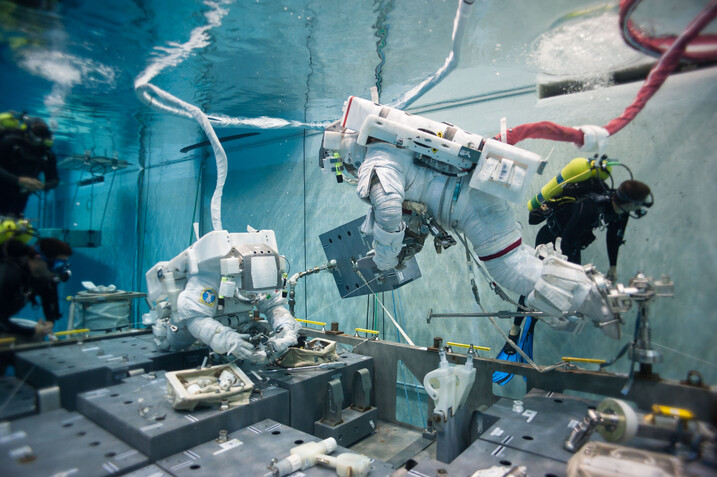
At the JSC, NASA trains astronauts in their neutral buoyancy lab (NBL)—essentially a large pool that simulates a weightless environment. Katherine McMann of the Aerospace Medicine program says that this preparation is critical for participation in the extravehicular activity (EVA) that is the cornerstone of space missions. That’s why the agency subjects trainees to a battery of tests to determine whether or not the trainees hearts and lungs can withstand the extended dives necessary for the simulation.
“While training at NBL, astronauts simulate EVAs in underwater dives that last multiple hours at a time,” McMann explains. “Diving is not without its risks. The change in pressure during ascent and descent increases the risk for pulmonary over-inflation, alveolar rupture, and cerebral air embolization. Thus, before diving, the health of potential divers is assessed to ensure they are physically capable to handle the stresses of diving.”
Akusobi’s job was to assess which tests yielded useful data and which did not.
“There are so many different parameters used in these tests,” he explains. “We found that one of them was not very effective or clinically useful. So, the recommendation that I made from my project was to drop a specific metric because it was not adding valid clinical information. That will help NASA to focus on the data that’s truly useful in assessing someone’s ability to engage in the training.”
The big takeaway for Akusobi was not the results of his research, but the people he met through the clerkship—new colleagues with whom he may reunite for future projects on space exploration.
“I met a lot of people who shared my interest in space and medicine,” he says. “I’ll continue to stay engaged and go to conferences. I hope at some point to collaborate with NASA on a project or even work for the agency. I would be excited to lend my expertise. This field is only getting bigger.”
McMann says Akusobi was “always engaged,” “extremely proactive,” and “an absolute pleasure to have as one of our top selected candidates” in the Aerospace Medicine Clerkship. “Chidi was truly an asset to the clerkship and I wouldn’t be surprised to see him in the aerospace medicine community in the future, should it be a part of his pursuits.”
As long as he can return safely to his family, Akusobi would like to experience space travel for himself some day. In the near future, though, his plans are more terrestrial: a residency in internal medicine and then a fellowship in a medicine subspeciality. His goal is to be a “committed physician-scientist” who connects clinical work with basic science, and vice versa. “I want to see patients in the hospital and also have a research program where I work on hard problems that will push medicine forward,” he says.
Consistent with the service ethic with which he grew up, Akusobi wants to reach beyond the hospital and laboratory. He says that, going forward, he hopes to make science communication a part of his career. In light of the recent pandemic, the need has never been greater for those who can help people understand science and medicine—and also inspire others like him to enter those fields.
“I want to talk to the public, especially when it comes to infectious diseases and vaccines,” he says. “I think there’s a lot of education that’s needed to get people on board with public health interventions and I want to be part of that conversation. I also want to inspire more Black and brown students to enter science and medicine. As I finish at Harvard and move onto the next phase of my career, I’m committed to being a mentor and role model in whatever way I can.”
This research was funded by the National Institute of Allergy and Infectious Diseases, and by the U.S. Department of Health and Human Services.
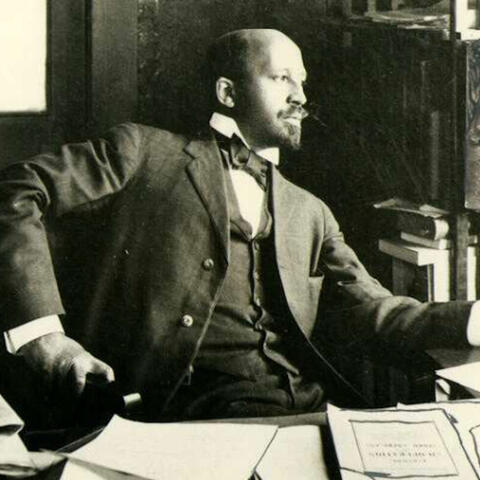
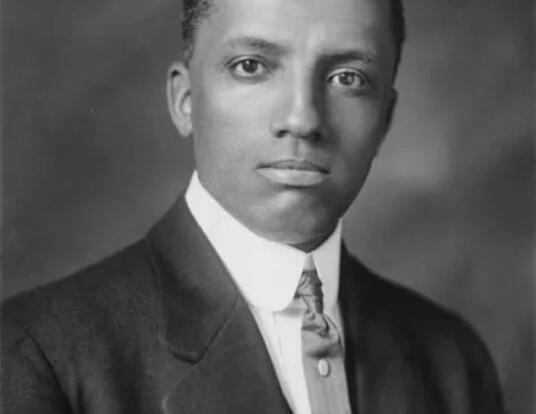
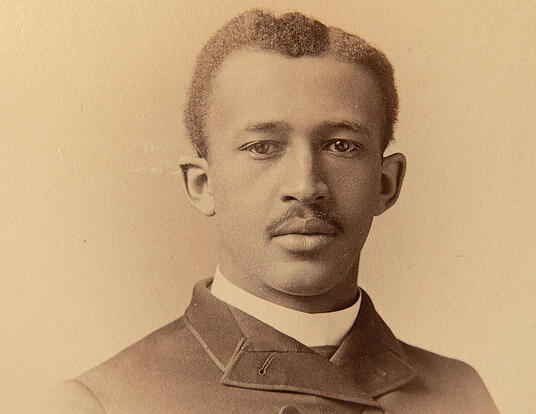
Photos by David Leifer and Courtesy of Wiki Commons
Get the Latest Updates
Join Our Newsletter
Subscribe to Colloquy Podcast
Simplecast